Brachial Plexus Blocks
The brachial plexus provides innervation to the bony structures and soft tissues of the upper extremity, and can be blocked in multiple anatomic positions. The interscalene, supraclavicular, and infraclavicular approaches are commonly used for a wide array of injuries and procedures. There are more approaches to blocking the brachial plexus but these are some of the most widely used.
Interscalene Brachial Plexus Block
Common Indications: Shoulder dislocation, proximal/mid-humerus fractures, deltoid laceration or abscess
Considerations & Technical Details
Considerations:
Use with caution in patients with respiratory issues as phrenic nerve paralysis is common. You should operate under the assumption that this block will anesthetize the phrenic nerve as it runs extremely close to the interscalene space.
As the neck is highly vascular, check your identified site with color doppler to identify small vessels that may overly the brachial plexus. As with all nerve blocks, a negative aspiration is essential before injecting anesthetic.
The interscalene block is most effective for the shoulder and proximal upper extremity. It will not reliably anesthetize the elbow, forearm, or hand.
Transducer: High-frequency linear probe
Needle: 18-22g 1.5-2in (3.8-5 cm) needle
Anesthetic volume: 10-15mL
Target of anesthetic: Vertical stack of cords between the anterior and medial scalene muscles (the interscalene space).
Positioning
Patient is supine or sitting up slightly with the head to the contralateral side. Transducer is placed 2-3cm superior to the midpoint of the clavicle, or slightly superior to the external jugular vein if it can be appreciated.
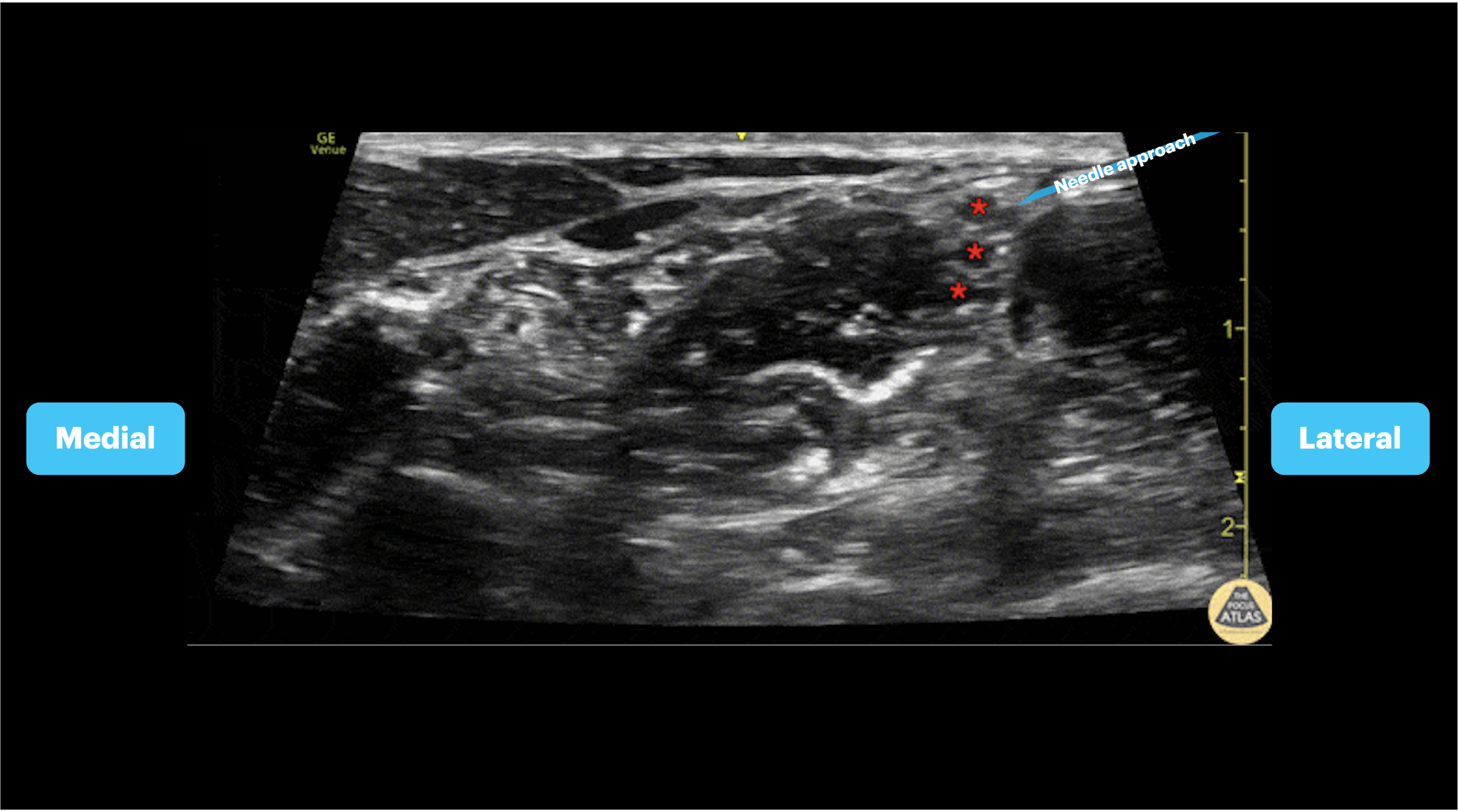
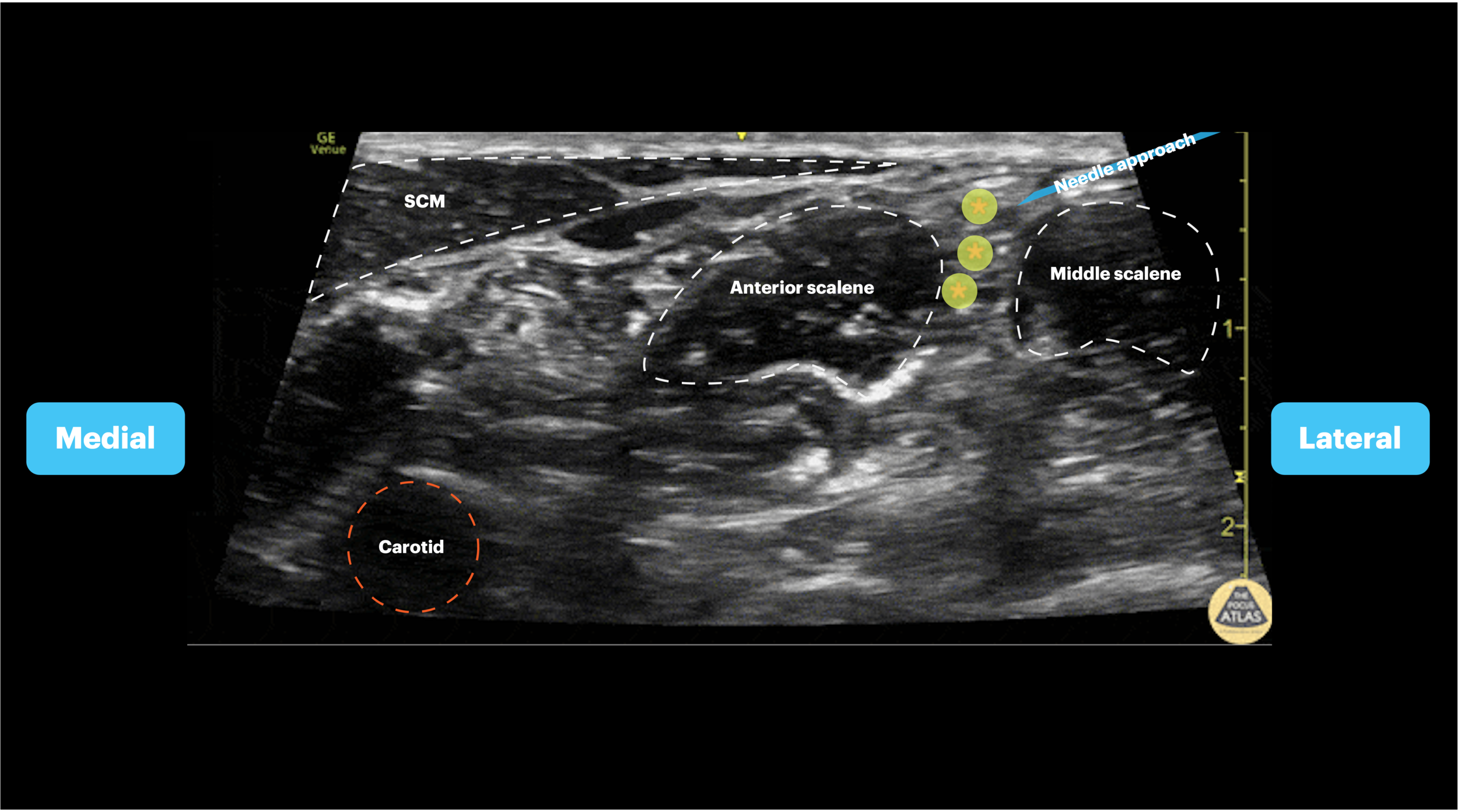
Target Identification
Two techniques can be used to identify the cords for the interscalene block. 1) The carotid artery can be identified deep to the sternocleidomastoid, then the probe can be slid posteriorly until a stack of cords is seen in between the anterior and middle scalenes. 2) Identify the subclavian artery in the supraclavicular fossa and trace the brachial plexus up into the interscalene space.
Needle Approach
Once this view is obtained, an in-plane approach should be used. The needle should be advanced from lateral to medial towards the vertical stack of cords between the anterior and middle scalene muscles (interscalene space).
Interscalene Blocks
Supraclavicular Brachial Plexus Block
Indications: Injury to the humerus, elbow, forearm and hand
Considerations & Technical Details
Considerations:
Phrenic nerve involvement is possible although less common than with the interscalene block.
As the neck is highly vascular, check your identified site with color doppler to identify small vessels that may overly the brachial plexus. As with all nerve blocks, a negative aspiration is essential before injecting anesthetic.
Ensure that the first rib is visualized under the subclavian artery and brachial plexus to avoid inadvertent pneumothorax.
Transducer: High-frequency linear probe
Needle: 18-22g 1.5-3.5 in (3.8-8.9 cm) needle
Anesthetic Volume: 20-25mL, generally a higher volume of anesthetic than interscalene as the trunks spread out widely in this region.
Target of Anesthetic: Anesthetic spread around the brachial plexus, peeling the plexus away from the rib and artery
Positioning
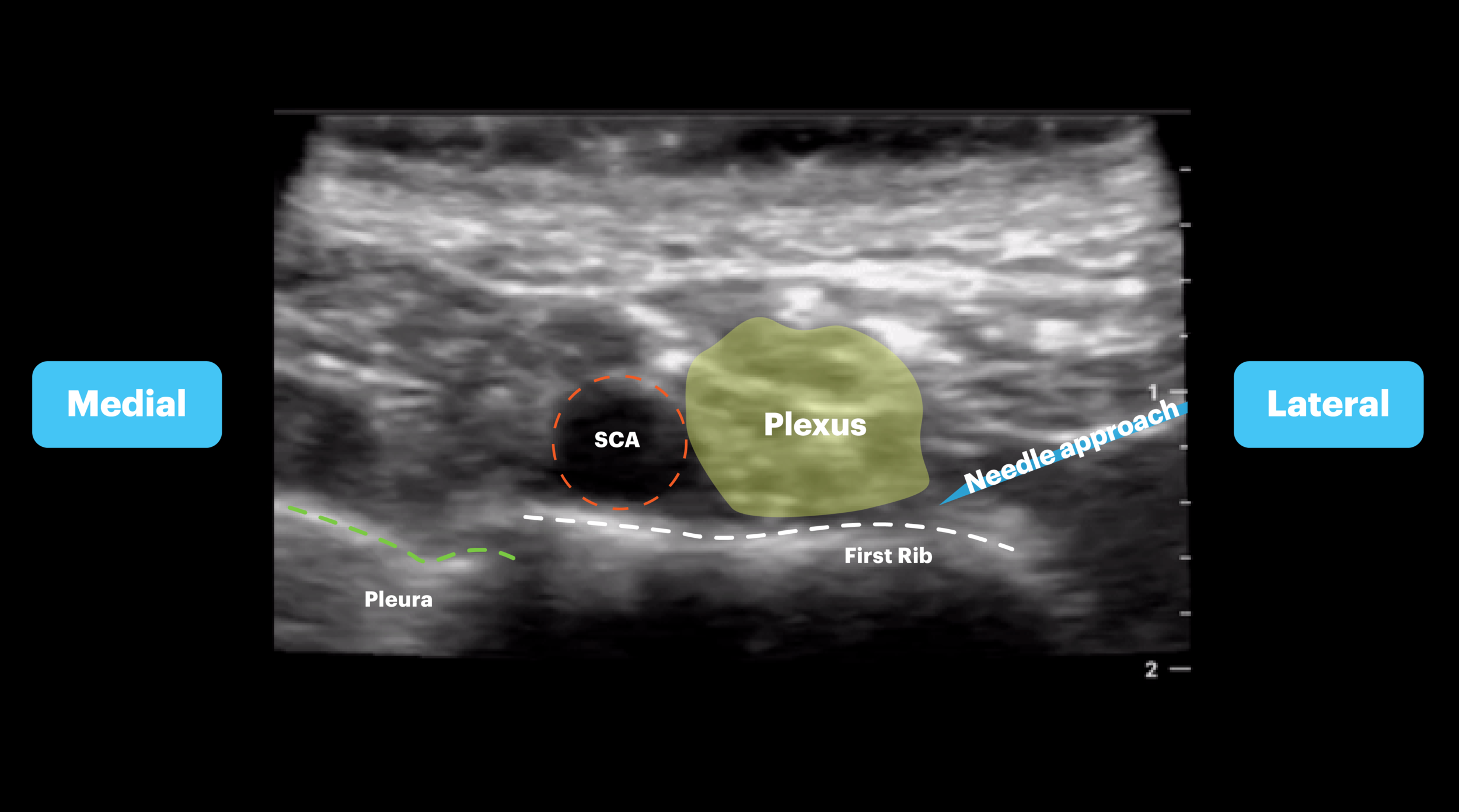
Patient is supine with head rotated to the contralateral side. The ipsilateral arm should be adducted and a roll can be placed under the scapula to open up the supraclavicular space. The probe is placed parallel to and just above the clavicle. Make sure to fan the transducer beam into the chest to improve visualization. Identify the first rib, subclavian artery and pleura.
Target Identification
Once you place the probe parallel to and just superior to the clavicle, fan the transducer beam into the chest and identify the pulsatile subclavian artery. Next you will want to identify the first rib as a hyperechoic line with posterior acoustic shadowing lying just deep to the artery. The pleura will be seen on one or two sides of the rib depending on your exact prone angle. The brachial plexus will lie just LATERAL to the artery at this location.
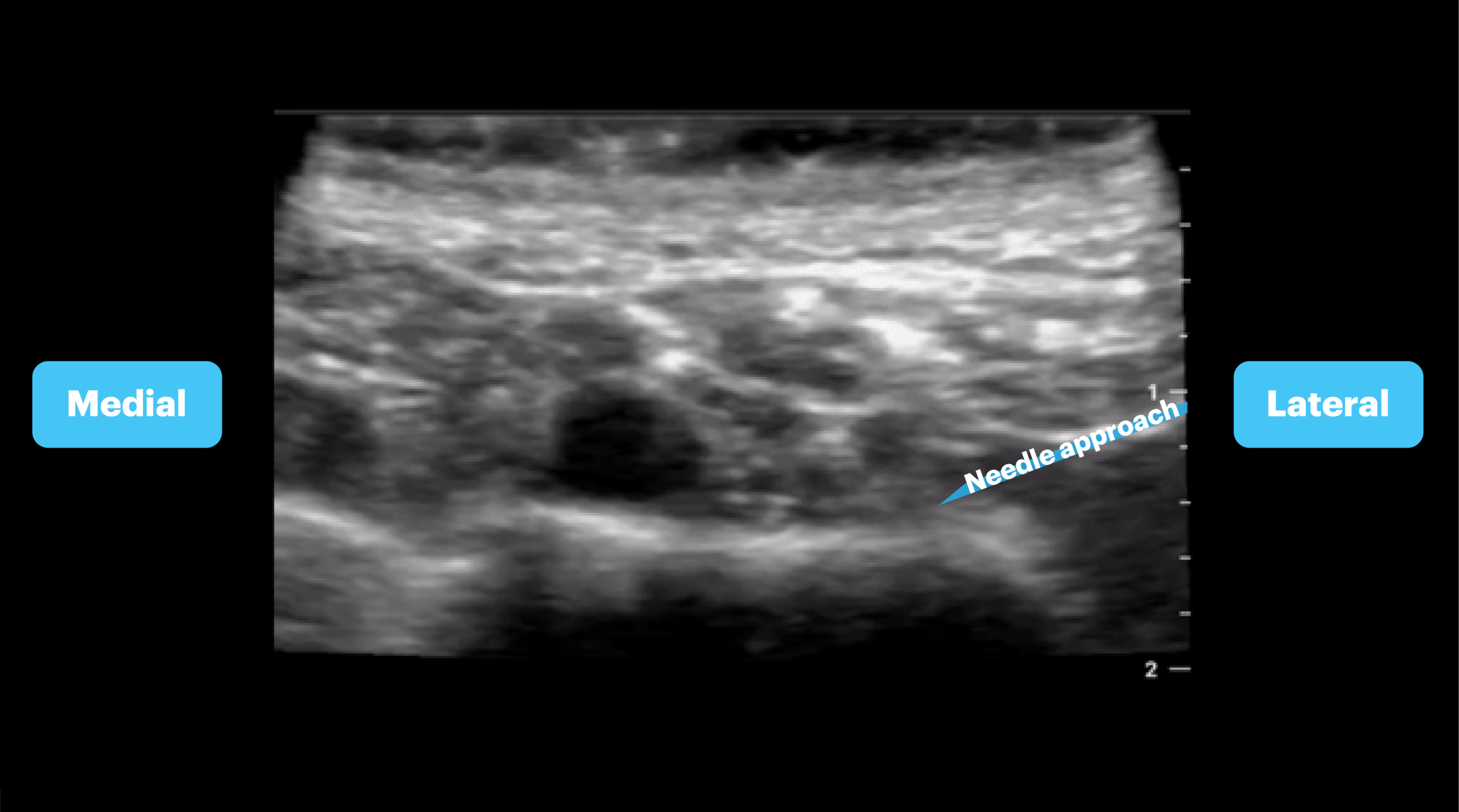
Needle Approach
Once this view is obtained, an in-plane approach should be used. The needle should be advanced from lateral to medial towards the plexus sheath. Stay outside the sheath and inject local anesthetic around the sheath to separate it from the first rib below.
Supraclavicular Blocks
Infraclavicular Brachial Plexus Block
Indications: Injuries of the upper arm, elbow, forearm, and hand
Considerations & Technical Details
Considerations:
The infraclavicular block does not anesthetize the shoulder.
As the neck is highly vascular and injection for this block occurs directly around the axillary artery, check your identified site with color doppler to identify small vessels that may overly the target site. As with all nerve blocks, a negative aspiration is essential before injecting anesthetic.
The brachial plexus cords may not always be clearly identified with this block, but injecting anesthetic to surround the axillary artery typically results in successful anesthesia.
Transducer: High-frequency linear probe
Needle: 18-22 g 3.5 in (8.9 cm) spinal needle
Anesthetic Volume: 20-25 mL
Target of Anesthetic: Local anesthetic spread deep to the axillary artery
Positioning
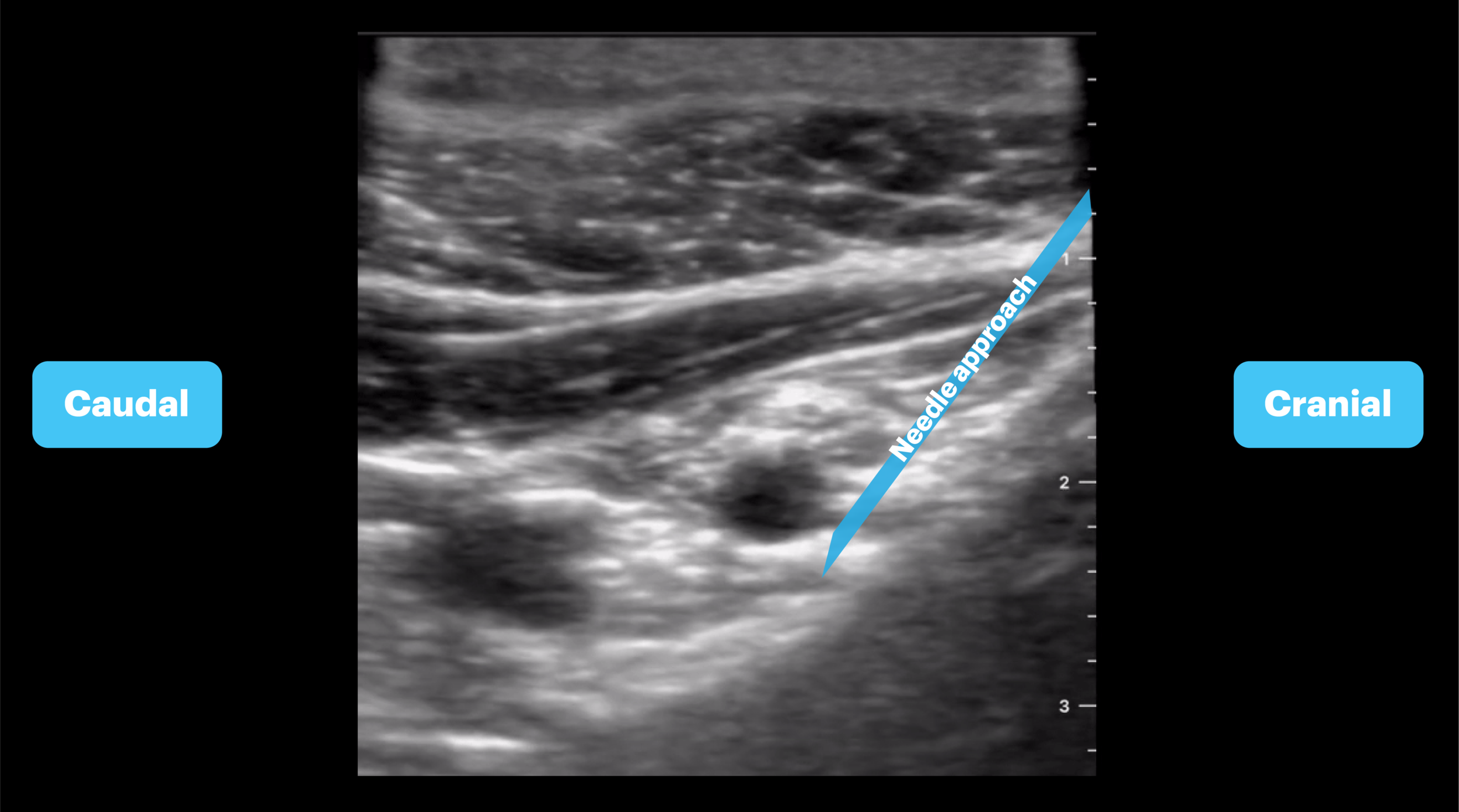
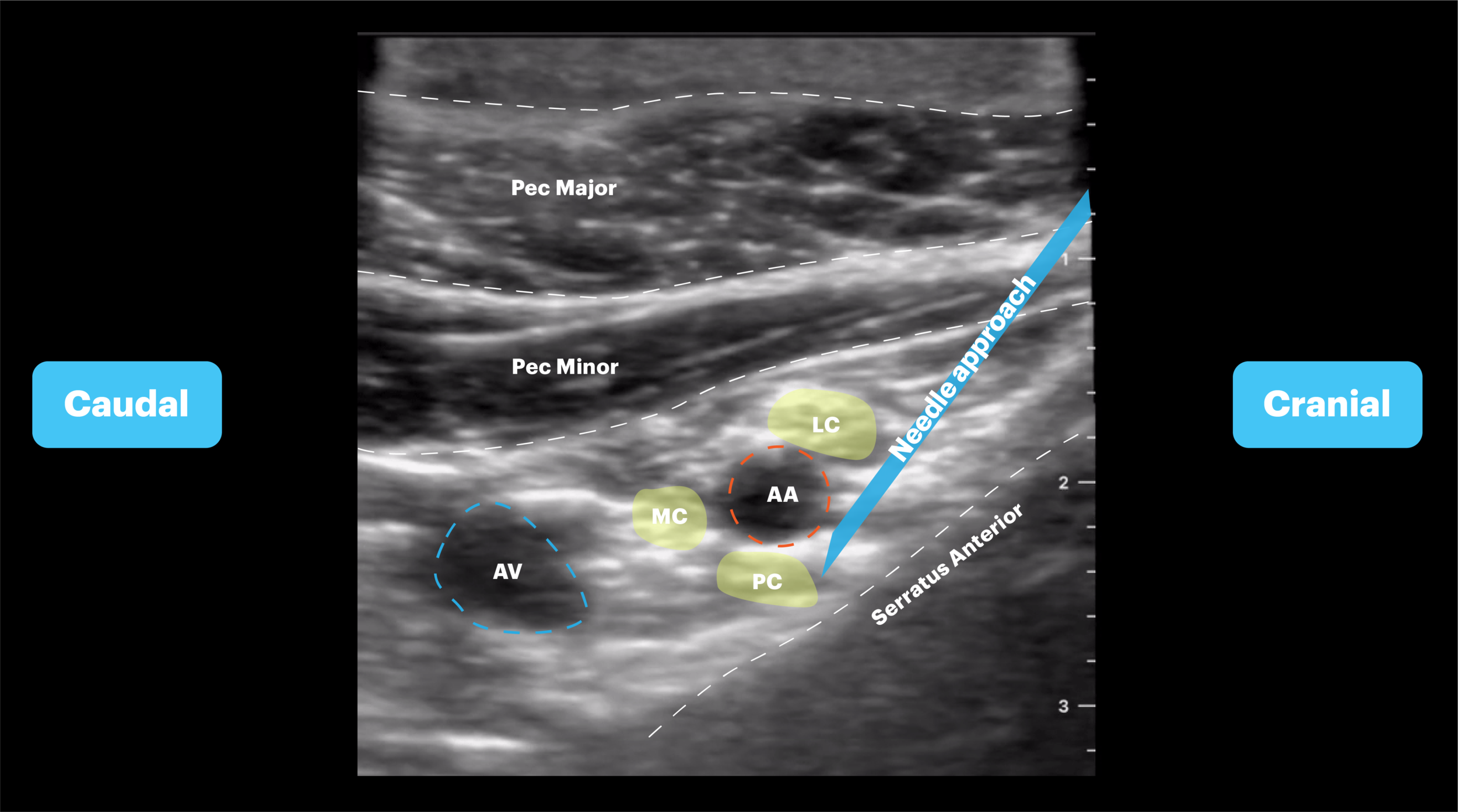
Patient is supine or sitting with head turned to contralateral side and the shoulder abducted to 90 degrees. The probe is placed in a parasagittal orientation just medial coracoid process and inferior to the clavicle.
Target Identification
It may be easiest to first palpate the coracoid process as this is a key landmark. Begin scanning just medial to the coracoid, keeping the probe in a sagittal orientation. Scan medially and laterally until you identify the axillary artery with surrounding brachial plexus cords. Be sure to identify the pleura posterior to the axillary artery. If pleura is seen you need to slide laterally until serratus anterior appears. This should be done to minimize risk of pneumothorax.
Needle Approach
The brachial plexus cords (lateral, medial, and posterior) surround the axillary artery in a variable pattern but cannot always be individually visualized. The goal is anesthetic spread around the axillary artery. Once this view is obtained, an in-plane approach should be used. The needle should be inserted just inferior to the clavicle and aimed caudal towards the posterior aspect of the axillary artery.