Lower Extremity Nerve Blocks
There are multiple nerve blocks that can be used to provide analgesia for the lower extremity. This includes the fascia iliaca compartment, popliteal sciatic, posterior tibial, and common peroneal nerve blocks. These blocks can be accomplished relatively easily using ultrasound given the superficial location of many of these nerves.
Fascia Iliaca Compartment Nerve Block
Indications: fractures of the femoral head, neck, intertrochanteric/subtrochanteric regions, shaft. Proximal tibial fractures. Anterior thigh lacerations or abscesses.
Considerations & Technical Details
Considerations:
Discuss with your consultant prior to performing the block and document a detailed neurovascular exam. Do not perform if there is a concern for compartment syndrome.
The fascia iliaca block is very similar to the femoral nerve block, but due to its plane block nature, will usually anesthetize the lateral femoral cutaneous nerve in addition to the femoral nerve. The injection of anesthetic distant from the neurovascular bundle also reduces the risk of intravascular injection and nerve injury.
Due to the large volume of this block, be sure to calculate a maximum safe dose of anesthetic (using an app such as SafeLocal or MDCalc). If needed, the anesthetic can be diluted 1:1 with normal saline to increase volume while avoiding toxicity.
Transducer: High-frequency linear probe
Needle: 18-22g 3.5 in (8.9cm) spinal needle
Anesthetic Volume: 20-40 mL
Target of Anesthetic: The space deep to the fascia iliaca and superficial to the iliacus muscle, lateral to the femoral neurovascular bundle.
Positioning
With the patient supine, place the probe in a transverse orientation just inferior to the inguinal crease, in the medial third of the inguinal crease. Identify the femoral artery with the nerve just lateral to it. Laterally, identify the iliacus muscle, with the sartorius muscle superior to this. The fascial plane between these muscles which surrounds the femoral nerve is the fascia iliaca.
More Examples
Transgluteal Sciatic Nerve Block
Indications: Sciatic nerve pain, injuries (burns, lacerations, abscesses) of the posterior thigh
Considerations and Technical Details
Considerations:
In addition to normal nerve block precautions; be aware that there is a ~6% risk of foot drop occurring and the patient should be made aware and encouraged not to drive for the duration of the block.
Transducer: Low-frequency curvilinear probe
Needle: 20-22 g 8-10cm Quincke or echogenic block needle (Needle visualization for deep targets is easier with an echogenic needle)
Anesthetic volume: 10-20 mL of long acting anesthetic.
Optional: Can add 4-8mg of dexamethasone
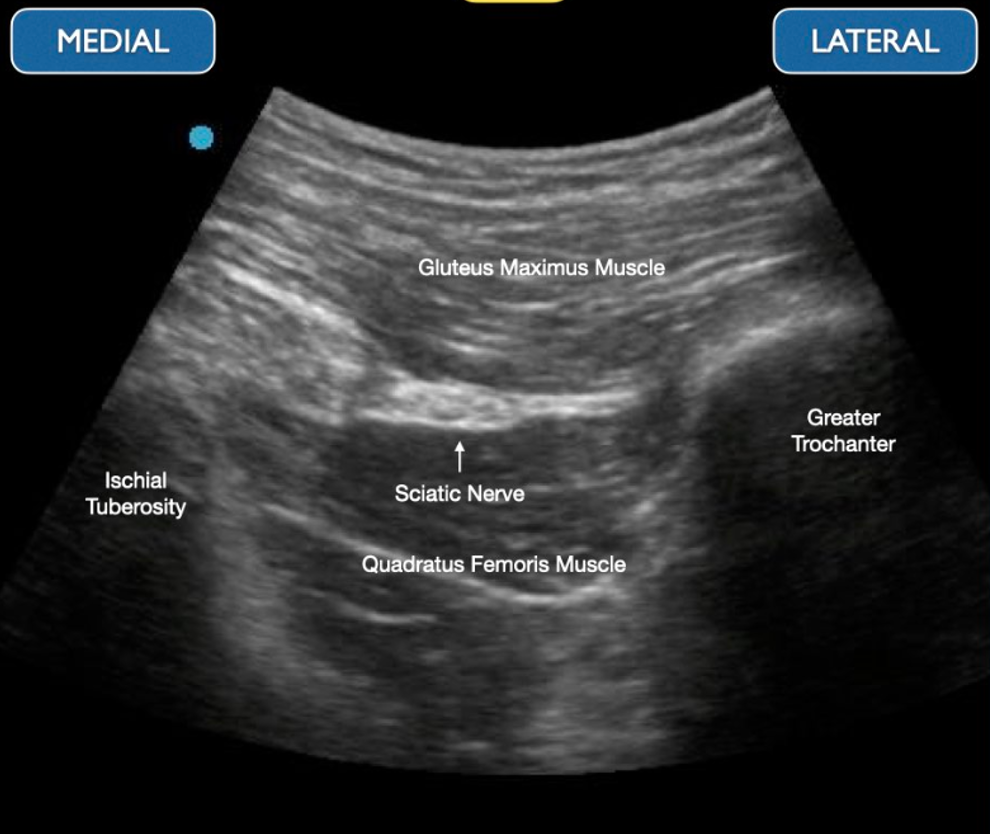
Target of Anesthetic: anesthetic spread around the sciatic nerve between the gluteus maximus and quadratus femoris muscle bellies.
Positioning
Position the patient in the decubitus position with the leg flexed at the hip and knee flexed for comfort. Palpate the greater trochanter laterally and posterior iliac spine medially. Position the curvilinear transducer along this line. Identify the greater trochanter and ischial tuberosity under ultrasound guidance. Note that for this block; a much steeper angle of approach is required and your needle should likely enter at 60 - 70 degrees.
More Examples
Popliteal Sciatic Nerve Block
Indications: distal tibia/fibula fractures, foot fractures, achilles tendon rupture, lower extremity burns, lacerations and I&Ds.
Considerations & Technical Details
Considerations:
Discuss with your consultant prior to performing the block, document a detailed neurovascular exam. Do not perform if there is concern for compartment syndrome.
Injecting around and not within Vloka’s sheath will not adequate anesthetize and requires needle repositioning.
Transducer: High-frequency linear probe
Needle: 20-22 g 1.5-2 in (3.8-5 cm) needle
Anesthetic volume: 10-20 mL
Target of Anesthetic: anesthetic spread around the sciatic nerve, within the sheath encompassing the sciatic nerve (Vloka’s sheath).
Positioning
With the patient in the lateral or prone position, place the transducer in a transverse orientation at the popliteal fossa. Identify the popliteal artery and vein. Superficial to these will be the branching distal segments of the sciatic nerve: the common peroneal nerve (CPN) and tibial nerve (TN). Trace these nerves proximally until they join into the sciatic nerve.
More Examples
Common Peroneal Nerve Block
Indications: laceration or abscess of lateral lower leg.
Considerations & Technical Details
Considerations:
Document a neurovascular exam prior to performing the block.
Transducer: High-frequency linear probe
Needle: 22-25g 1.5-2 in (3.8-5 cm) needle
Anesthetic volume: 4-5 mL
Target of Anesthetic: Anesthetic spread around common peroneal nerve just superficial to the fibular head
Positioning
Position the patient supine or in contralateral decubitus. Place the probe in a transverse orientation just inferior to the fibular head on the lateral aspect of the proximal lower leg. Identify the common peroneal nerve just superficial to the fibular cortex.
More Examples
Posterior Tibial Nerve Block
Indications: wound exploration, lacerations, and/or foreign body removal on the sole of the foot, calcaneal fractures
Considerations & Technical Details
Considerations:
If the tibial nerve and artery are too close together, one can slide proximally to separate these structures.
Transducer: High-frequency linear probe
Needle: 23-27g 1-1.5 in (2.5-3.8 cm) needle
Anesthetic volume: 4-5 mL
Target of Anesthetic: Anesthetic spread around posterior tibial nerve with adjacent vascular bundle.
Positioning
Position the patient with slight external hip rotation and knee flexion to expose the medial malleolus. Place the probe posterior to the medial malleolus in a transverse orientation, and identify the tibial artery/vein using doppler flow. The posterior tibial nerve will be found lateral/posterior to the vascular bundle.